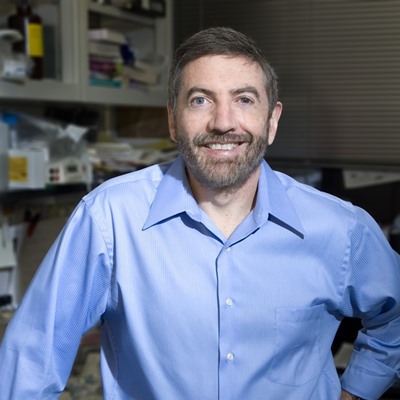

Dr. Glimcher is the Stephen and Suzanne Weiss Dean of Weill Cornell Medical College in New York. Previous to her current positions, she was the Irene Heinz Given Professor of Immunology at the Harvard School of Public Health, where she was director of the Division of Biological Sciences, and Professor of Medicine at Harvard Medical School, where she headed the immunology program. She also served as Senior Physician and Rheumatologist at the Brigham and Women's Hospital. As an immunologist, her primary research interests are elucidating the molecular pathways that regulate the immune system, critical for both the development of protective immunity and for the pathophysiologic immune responses underlying autoimmune, infectious and malignant diseases. She is a Fellow of the American Academy of Arts and Sciences, a Member of the National Academy of Medicine and a Member of the National Academy of Sciences. She sits on the Board of Trustees of Cornell University, the Board of Overseers of Weill Cornell Medical College, and the Board of Trustees of Memorial Sloan Kettering Cancer Center and is on the Corporate Board of Directors of the Bristol-Myers Squibb Pharmaceutical Corporation and the Waters Corporation.
Dr. Glimcher speaks nationally and internationally on rheumatology, immunology, skeletal biology and translational medicine and has contributed more than 350 scholarly articles and papers to the medical literature.
ER stress sensors in disease
The endoplasmic reticulum (ER) is a key intracellular organelle that performs multiple physiological functions such as protein folding, post-translational modification, fatty acid and sterol biosynthesis, detoxification of xenobiotics, and the storage of intracellular calcium. The mammalian stress sensor IRE1α plays a central role in the unfolded protein or endoplasmic reticulum (ER) stress response by activating its downstream transcription factor XBP1 via an unconventional splicing mechanism. IRE1α can also induce the degradation of a subset of mRNAs in a process termed regulated IRE1-dependent decay (RIDD). Our studies in the last several years have sought to explore the in vivo function of this signaling pathway using genetically manipulated rodent models coupled with transcriptomic and biochemical analyses. Ablation of IRE1α or XBP1 caused severe abnormalities in exocrine and endocrine pancreatic acinar cells, plasma B cells, zymogenic Paneth cells and Chief cells in the gastrointestinal tract, manifested by failure of ER expansion, reduced production of secretory proteins, and increased apoptosis. Silencing of XBP1 improves survival in several mouse models of neurodegenerative diseases. We recently described an unsuspected new function for the XBP1 transcription factor in mammalian host defenses and in cancer immunotherapy. Our most recent data on the function of IRE1/XBP1 in cancer and in the immune system will be presented.